Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
Balancing Weight Loss and Morality: The Ethical Considerations of Bariatric Balloons in Healthcare
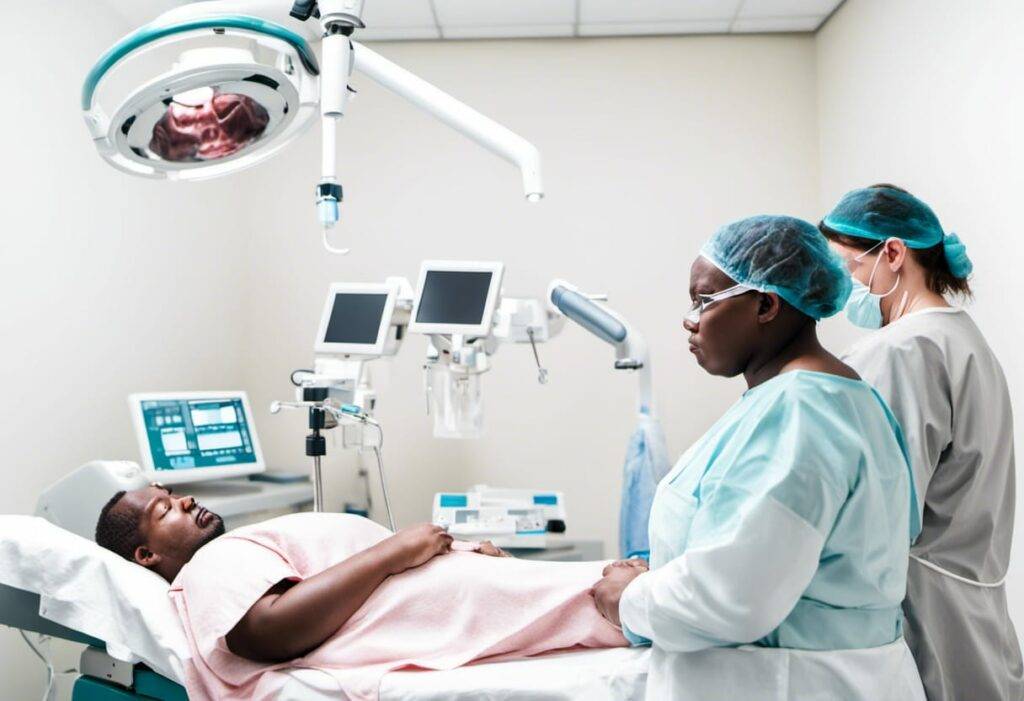
Achieving weight loss is a complex journey that often requires a multifaceted approach. For some individuals struggling with obesity, a bariatric balloon may be a morally upright solution. This article explores the circumstances in which a morally upright healthcare provider would advocate for the use of a bariatric balloon as a strategy for weight loss. We will delve into the terminology, underlying principles, ethical considerations, potential risks, and benefits associated with this procedure. Through evidence-based research, we aim to present a clear and accessible exploration of the ethical framework guiding the use of bariatric balloons in weight management.
Understanding Bariatric Balloons:
A bariatric balloon, also known as an intragastric balloon, is a temporary, non-surgical procedure that involves placing a balloon in the patient’s stomach to promote weight loss. This treatment option is typically considered when lifestyle changes alone have not yielded satisfactory weight loss results. It is essential to note that bariatric balloons are not a standalone solution but rather a tool that assists individuals in achieving weight loss goals.
Ethical Considerations:
1. Respect for Autonomy: A morally upright healthcare provider must respect the autonomy of the patient when discussing the use of a bariatric balloon. The individual’s consent and comprehension of the procedure, including potential risks and benefits, are of utmost importance. Open and honest communication ensures that the patient makes an informed decision.
2. Beneficence: The principle of beneficence obligates healthcare providers to act in the best interest of the patient. For individuals with severe obesity and related comorbidities, a bariatric balloon may offer a preliminary step towards weight reduction, promoting overall health improvements and potentially reducing the risk of other medical conditions.
3. Non-maleficence: Healthcare providers must weigh the potential risks of the procedure against the expected benefits. While bariatric balloons are generally considered safe, there are associated risks such as gastric ulcers, balloon deflation, and complications related to the insertion and removal process. A thorough evaluation of the patient’s medical history and informed consent is vital to minimize potential harm.
4. Justice: The principle of justice emphasizes the fair distribution of healthcare resources. In advocating for the use of a bariatric balloon, healthcare providers must consider whether this intervention aligns with equitable access to care. It is crucial to assess whether the procedure is deemed necessary compared to other available weight loss options and consider potential disparities in its availability.
Considerations Before Committing to the Procedure:
1. Comprehensive Evaluation: Prior to committing to a bariatric balloon procedure, patients must undergo a thorough evaluation. This evaluation includes an assessment of their medical history, current body mass index (BMI), comorbidities, psychological readiness, and willingness to adopt lifestyle changes in the long term.
2. Dietary Modifications: Weight loss achieved with a bariatric balloon procedure is most effective when combined with dietary modifications. A morally upright healthcare provider will emphasize the importance of a balanced, nutrient-rich diet and encourage patients to work with a registered dietitian to develop a personalized meal plan.
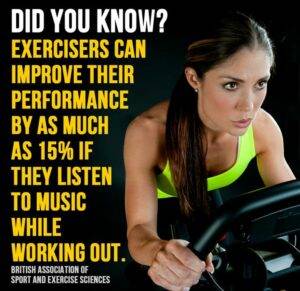
3. Commitment to Lifestyle Changes: A bariatric balloon serves as a temporary aid for weight loss. Patients must understand that long-term success relies on adopting and maintaining healthier lifestyle habits. Exercise, stress management, and behavior change strategies should be integral components of the patient’s weight loss journey.
4. Psychological Support: Weight loss can be mentally challenging for individuals struggling with obesity. A morally upright healthcare provider recognizes the importance of providing psychological support through counseling, support groups, or referrals to mental health professionals.
Benefits and Potential Risks:
1. Benefits:
– Facilitates initial weight loss: Bariatric balloons may help individuals kick-start their weight loss journey by creating a feeling of fullness, leading to reduced calorie intake.
– Improves overall health: Weight loss achieved through bariatric balloons may reduce the risk of obesity-related comorbidities such as type 2 diabetes, high blood pressure, and sleep apnea.
– Motivates lifestyle changes: The initial weight loss experienced with a bariatric balloon can serve as a motivational boost, encouraging individuals to continue making healthier choices.
2. Potential Risks:
– Gastric ulcers: A small percentage of individuals may develop gastric ulcers as a result of constant contact between the balloon and the stomach lining.
– Balloon deflation: Rare instances of balloon deflation may occur due to perforation or leakage, necessitating immediate medical attention.
– Insertion and removal risks: As with any medical procedure, the insertion and removal of the bariatric balloon carry inherent risks, such as infection or injury to surrounding tissues.
Balancing Ethics and Weight Management:
A morally upright healthcare provider will consider bariatric balloons as a potential weight loss tool for individuals who have exhausted other conservative measures without significant success. It is essential to approach each patient with empathy, ensuring they are fully informed about the procedure’s risks, benefits, and long-term implications. By emphasizing patient autonomy, beneficence, non-maleficence, and justice, healthcare professionals can navigate the ethical considerations associated with bariatric balloons.
While I do cite reputable sources, I am not a medical professional. Please use professional medical advice when making any health-related decisions.
Conclusion:
Utilizing a bariatric balloon as a weight loss aid requires careful consideration, incorporating both ethical principles and patient-specific factors. The temporary nature of bariatric balloons necessitates comprehensive lifestyle modifications to achieve sustainable weight loss. Engaging in open discussions, providing thorough evaluations, and offering ongoing support are imperative to address the ethical dimensions of this procedure. By conscientiously factoring in the wellness and autonomy of the individual, healthcare providers can responsibly advocate for the use of bariatric balloons as part of a morally upright approach to weight management.
Reputable Sources:
1. American Society for Metabolic and Bariatric Surgery (ASMBS). “Intragastric Balloon.” https://asmbs.org/patients/bariatric-surgery-procedures/intragastric-balloon
2. National Institute for Health and Care Excellence (NICE). “Obesity: identification, assessment, and management.” https://www.nice.org.uk/guidance/ng189/chapter/Recommendations
3. Mayo Clinic. “Intragastric balloon.” https://www.mayoclinic.org/tests-procedures/intragastric-balloon/about/pac-20393995
4. Obesity Action Coalition (OAC). “Intragastric Balloons.” https://www.obesityaction.org/community/article-library/intragastric-balloons-in-the-treatment-of-morbid-obesity/
5. Genco, A., Bruni, T., & Koppman, J. (2017). “Intragastric Balloon for Obesity Treatment: Results of a Multicenter Study on 3266 Patients.” Obesity Surgery, 27(2), 327-332.

Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.