Are you struggling to understand the complexities of obesity and its impact on your health? Look no further! In this comprehensive blog post, we have compiled the top 30 medical questions about obesity that adults often ask. From understanding the causes and risks, to finding effective treatment options, we have got you covered. Whether you’re a health enthusiast, medical professional, or someone looking for answers, this post will provide all the information you need. So, let’s dive into the depths of obesity and emerge with a better understanding of this pressing health concern.
Discover the Truth About Obesity: What Every Adult Should Know
1. What is obesity and how is it defined in medical terms?
Obesity is a medical condition characterized by the excessive accumulation and storage of fat in the body. It is typically diagnosed using body mass index (BMI), which is a measure of body fat based on height and weight. In medical terms, obesity is defined as having a BMI of 30 or higher. BMI is calculated by dividing a person’s weight in kilograms by their height in meters squared. For example, a person who is 1.7 meters tall and weighs 90 kilograms would have a BMI of 31.
The significance of this question is that it provides a clear understanding of what obesity is and how it is medically defined. This understanding forms the basis for further discussions on the causes, consequences, and management of obesity.
2. Are genetics a major factor in the development of obesity?
Genetics can play a role in the development of obesity, but it is generally agreed upon that environmental factors, such as diet and physical activity, have a larger influence. Several studies have shown that genetics can contribute to a person’s susceptibility to obesity, with heritability estimates ranging from 40-70%. However, the specific genes and mechanisms involved are complex and not fully understood.
The significance of this question is that it helps to debunk the common misconception that obesity is solely determined by genetics. By highlighting the importance of environmental factors, such as lifestyle choices, it empowers individuals to make positive changes to prevent or manage obesity.
3. What are the common causes of obesity in adults?
The common causes of obesity in adults are multifactorial and include a combination of genetic, environmental, and behavioral factors. These factors can include a sedentary lifestyle, unhealthy dietary choices, cultural influences, socioeconomic status, psychological factors (such as stress and depression), and certain medical conditions (such as hypothyroidism or polycystic ovary syndrome).
Studies have consistently shown that increased consumption of energy-dense foods, high in sugars and fats, combined with reduced physical activity, are primary contributors to adult obesity. For example, a meta-analysis of 88 studies found that a higher intake of sugar-sweetened beverages was associated with a higher risk of obesity.
The significance of this question is that it sheds light on the multiple factors that contribute to obesity in adults. Understanding these causes is crucial for developing effective prevention and treatment strategies.
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.
4. How does obesity affect overall health and increase the risk of other diseases?
Obesity has significant implications for overall health and increases the risk of various diseases. It is associated with a higher prevalence of cardiovascular diseases (such as coronary heart disease and stroke), type 2 diabetes, certain types of cancer (such as breast, colorectal, and endometrial cancer), musculoskeletal disorders, sleep apnea, and mental health conditions (such as depression and anxiety).
One large cohort study, known as the Global BMI Mortality Collaboration, analyzed data from239 studies involving more than10 million participants. It found that higher BMI was positively associated with an increased risk of all-cause mortality, as well as specific causes of death such as cardiovascular diseases, cancer, and respiratory diseases.
The significance of this question is that it highlights the seriousness of obesity as a health condition. It emphasizes the need for prevention, early detection, and management of obesity to reduce the risk of associated diseases and improve overall health outcomes.
5. Are there different types or classifications of obesity?
Obesity can be classified into different types based on factors such as body fat distribution and underlying medical conditions. One commonly used classification is based on body fat distribution and distinguishes between android obesity (more fat around the abdomen) and gynoid obesity (more fat around the hips and thighs).
Another classification system is based on the presence of underlying medical conditions, such as obesity-related metabolic disorders. This includes conditions such as metabolic syndrome, which is a cluster of risk factors (including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat) that often co-occur with obesity.
The significance of this question is that it recognizes the heterogeneity of obesity and emphasizes the importance of personalized approaches to its prevention and management. It also highlights that different types or classifications of obesity may have different health implications.
6. How does obesity impact mental health and emotional well-being?
Obesity can have significant impacts on mental health and emotional well-being. It is associated with an increased risk of depression, anxiety, poor self-esteem, and body dissatisfaction. These psychological effects can further contribute to unhealthy eating behaviors, social isolation, and a decreased quality of life.
A systematic review and meta-analysis of 15 longitudinal studies found that obesity in childhood and adolescence was associated with an increased risk of developing depression in adulthood.
The significance of this question is that it recognizes the importance of addressing mental health and emotional well-being in individuals with obesity. It highlights the need for comprehensive approaches that address both physical and mental health aspects of obesity.
7. Can certain medications contribute to weight gain or obesity?
Yes, certain medications can contribute to weight gain or obesity. Common examples include certain antidepressants (such as selective serotonin reuptake inhibitors), antipsychotics, corticosteroids (used for conditions like asthma or arthritis), and some medications used to treat epilepsy or diabetes.
The significance of this question is that it highlights the potential impact of medications on weight and emphasizes the importance of considering the potential side effects when prescribing medications, especially in individuals who are already at risk for obesity.
8. What are the health risks associated with obesity, such as cardiovascular diseases and diabetes?
Obesity is associated with an increased risk of various health conditions, including cardiovascular diseases (such as heart disease, hypertension, and stroke), type 2 diabetes, certain types of cancer, musculoskeletal disorders (such as osteoarthritis), sleep apnea, and non-alcoholic fatty liver disease.
One study, known as the Global Burden of Disease Study, estimated that in 2017, high BMI contributed to 4 million deaths globally, with cardiovascular diseases being the leading cause of death.
The significance of this question is that it highlights the specific health risks associated with obesity, which reinforces the importance of prevention, early detection, and management of obesity to reduce the burden of these diseases on individuals and society.
9. Can obesity affect fertility and pregnancy outcomes in women?
Obesity can have significant effects on fertility and pregnancy outcomes in women. It is associated with an increased risk of infertility, irregular menstrual cycles, and hormonal imbalances. Obesity can also increase the risk of complications during pregnancy, such as gestational diabetes, high blood pressure, pre-eclampsia, cesarean delivery, and fetal macrosomia (abnormally large birth weight).
A systematic review and meta-analysis of 39 studies found that obesity was associated with a higher risk of infertility and a lower chance of achieving a live birth after assisted reproductive technologies.
The significance of this question is that it recognizes the potential reproductive and pregnancy-related consequences of obesity in women. It underscores the importance of maintaining a healthy weight before and during pregnancy to optimize fertility and improve pregnancy outcomes.
10. What role does physical activity and exercise play in preventing and treating obesity?
Physical activity and exercise play a crucial role in both preventing and treating obesity. Regular physical activity helps to increase energy expenditure, build muscle mass, improve insulin sensitivity, and promote overall health. It can also help to maintain weight loss and prevent weight regain after initial weight loss.
A comprehensive review of the scientific literature on physical activity and obesity prevention found that higher levels of physical activity were associated with a lower risk of developing obesity. Additionally, a randomized controlled trial, known as the Look AHEAD study, found that individuals with type 2 diabetes who participated in an intensive lifestyle intervention, including increased physical activity, had greater weight loss compared to those in the control group.
The significance of this question is that it emphasizes the importance of physical activity and exercise as key components of obesity prevention and management. It highlights the need for promoting and facilitating regular physical activity at individual, community, and societal levels.
11. Is there a specific diet that can aid in weight loss and manage obesity?
While there is no one-size-fits-all diet for weight loss and managing obesity, several well-researched diets have shown positive effects. One such diet is the Mediterranean diet, which emphasizes whole grains, fruits, vegetables, lean proteins, and healthy fats while limiting processed foods and added sugars. Studies have found that adherence to the Mediterranean diet is associated with lower obesity rates and improved weight management.
Another effective diet for weight loss is a low-carbohydrate diet, such as the ketogenic diet. This diet restricts carbohydrates and encourages higher intake of fats and proteins. Research has shown that low-carbohydrate diets can lead to more significant weight loss and improvements in obesity-related health markers like insulin resistance and blood lipid levels.
The DASH (Dietary Approaches to Stop Hypertension) diet is also beneficial for weight loss and obesity management. It emphasizes a high intake of fruits, vegetables, whole grains, lean proteins, and low-fat dairy products while reducing sodium and saturated fats. The DASH diet has been shown to help with weight loss, reduce blood pressure, and improve overall cardiovascular health.
The significance of this question lies in the fact that dietary interventions are vital for weight management and preventing obesity-related health complications. Different diets can have varying effects on individuals, so it’s important to choose an approach that suits an individual’s preferences, health status, and lifestyle factors. Consulting with a healthcare professional or registered dietitian is recommended for personalized guidance.
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.
12. How does stress and psychological factors contribute to obesity?
Stress and psychological factors can contribute to obesity through various mechanisms. One primary way is through the consumption of high-calorie, unhealthy foods in response to stress or emotional triggers. This is often referred to as “emotional eating” or “comfort eating.” When stressed, individuals may turn to food as a coping mechanism, leading to overeating and weight gain.
Research has found that chronic stress can also alter the body’s hormonal balance, leading to increased appetite and a preference for energy-dense foods. Stress triggers the release of cortisol, a hormone associated with increased hunger and cravings for unhealthy foods.
Psychological factors, such as depression and anxiety, can also contribute to obesity. These mental health conditions may lead to decreased physical activity, poor eating habits, and medication side effects that promote weight gain.
The significance of understanding the link between stress, psychological factors, and obesity is crucial for developing effective weight management strategies. Addressing psychological factors, including stress management, emotional regulation, and psychological support, is essential alongside dietary and physical activity interventions for sustainable weight loss and obesity prevention.
13. Can certain medical conditions or hormonal imbalances cause obesity?
Certain medical conditions and hormonal imbalances can contribute to obesity. One such example is hypothyroidism, a condition where the thyroid gland does not produce enough thyroid hormones. Hypothyroidism can decrease metabolism and lead to weight gain.
Polycystic ovary syndrome (PCOS) is another condition that can cause obesity. PCOS is a hormonal disorder that affects the ovaries, resulting in irregular menstrual cycles, excess androgen production, and insulin resistance. Insulin resistance can lead to weight gain and difficulty losing weight.
Additionally, Cushing’s syndrome, a disorder characterized by high levels of the hormone cortisol, can also cause obesity. Excess cortisol can increase appetite, promote fat deposition, and redistribute fat to the abdominal area.
Understanding the role of medical conditions and hormonal imbalances in obesity is crucial for accurate diagnosis and appropriate treatment. Medical evaluation, including blood tests and hormone level assessments, is necessary to identify and address any underlying conditions contributing to obesity.
14. Is there a link between childhood obesity and long-term health issues in adulthood?
Yes, there is a strong link between childhood obesity and long-term health issues in adulthood. Numerous studies have highlighted the adverse health consequences of childhood obesity that persist into adulthood.
Childhood obesity increases the risk of developing several chronic conditions in adulthood, including type 2 diabetes, cardiovascular diseases, hypertension, dyslipidemia, and non-alcoholic fatty liver disease. Obesity in childhood also predicts a higher likelihood of remaining obese in adulthood, further exacerbating the risks associated with obesity-related health issues.
One long-term study, the Bogalusa Heart Study, followed children from childhood into their middle age. The study found that obese children often carried their weight into adulthood and had an increased risk of developing heart disease, diabetes, and other health problems later in life.
Addressing childhood obesity is crucial for preventing long-term health complications in adulthood. Early interventions focused on promoting healthy eating habits, physical activity, and overall lifestyle modifications can help reduce the risk of obesity-related chronic diseases later in life.
15. Can obesity be reversed or is it a lifelong condition?
Obesity can be reversed through sustainable lifestyle changes, including dietary modifications, increased physical activity, and behavior modifications. Numerous studies have demonstrated significant weight loss and improvements in health outcomes through lifestyle interventions.
One notable study, the Diabetes Prevention Program, showed that individuals at high risk for developing type 2 diabetes who achieved a 7% weight loss through lifestyle changes reduced their risk of developing diabetes by 58%.
Weight loss achieved through bariatric surgery has also been shown to result in long-term weight reduction and improved obesity-related health conditions. Meta-analyses of studies on bariatric surgery have reported sustained weight loss and remission of obesity-related comorbidities, such as type 2 diabetes and hypertension.
While obesity can be reversed, it requires ongoing commitment to maintaining a healthy lifestyle and managing weight. It is essential to recognize that managing obesity may be a lifelong endeavor for many individuals. Regular follow-up with healthcare professionals, including dietitians and exercise specialists, can provide necessary support and guidance for successful long-term weight management.
16. What are the surgical options available for weight loss in individuals with obesity?
Several surgical options are available for weight loss in individuals with obesity. The most commonly performed weight loss surgeries are gastric bypass, sleeve gastrectomy, and adjustable gastric banding.
Gastric bypass surgery involves creating a smaller stomach pouch and bypassing a portion of the small intestine, resulting in reduced food intake and nutrient absorption. Sleeve gastrectomy involves removing a large part of the stomach, creating a smaller stomach sleeve, which limits food intake and decreases hunger hormones. Adjustable gastric banding involves placing an inflatable band around the upper part of the stomach to create a small pouch, restricting food intake.
These surgical procedures result in significant weight loss and improvements in obesity-related health conditions, such as type2 diabetes, hypertension, and sleep apnea. Several studies have shown that bariatric surgery leads to sustained weight loss, improved quality of life, and long-term remission of obesity-related comorbidities.
However, it is important to note that weight loss surgeries are not without risks and complications. Potential complications include infection, bleeding, nutritional deficiencies, and issues related to the placement of the adjustable gastric band. Therefore, careful patient selection, comprehensive preoperative evaluation, and postoperative monitoring are necessary to ensure successful outcomes.
17. How effective are weight loss medications in treating and managing obesity?
Weight loss medications can be effective as part of a comprehensive approach for treating and managing obesity, particularly when used in conjunction with lifestyle modifications. Several medication options have been approved by regulatory bodies, such as the U.S. Food and Drug Administration (FDA), for long-term treatment of obesity.
Phentermine, for example, is an FDA-approved medication that suppresses appetite and is typically prescribed for short-term use in conjunction with lifestyle changes. Other medications, like orlistat, work by blocking the absorption of dietary fats in the intestines, leading to weight loss.
Studies have shown that weight loss medications, when combined with lifestyle interventions, can lead to more significant weight loss compared to lifestyle interventions alone. For instance, a study published in the New England Journal of Medicine found that individuals who received a combination of the medication liraglutide with lifestyle interventions achieved greater weight loss compared to those who received a placebo.
It is worth noting that weight loss medications should be used under the supervision of healthcare professionals, and the potential benefits and risks should be carefully evaluated on an individual basis. Lifestyle modifications, such as adopting a healthy diet and increasing physical activity, should remain the foundation of any weight loss or obesity management approach.
18. Can obesity be prevented? If so, what are the most effective prevention strategies?
Obesity can be prevented through a combination of lifestyle modifications and public health strategies. Multiple studies have highlighted the effectiveness of different prevention strategies in reducing the risk of obesity.
Effective prevention strategies include promoting a healthy diet that emphasizes whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, while reducing the consumption of processed and sugary foods. Encouraging regular physical activity across all age groups and reducing sedentary behaviors, such as excessive screen time, are also crucial components of prevention.
Additionally, creating supportive environments that ease access to healthy foods and safe spaces for physical activity can significantly contribute to obesity prevention. Policies aimed at reducing marketing of unhealthy foods to children, implementing taxation policies on sugary beverages, and creating walkable communities with access to parks and recreational facilities have shown promising results in obesity prevention.
The significance of prevention strategies lies in the fact that obesity is a complex and multifactorial issue. Preventing obesity is not only essential for reducing individual health risks but also for alleviating the burden on healthcare systems and society as a whole. A comprehensive and multifaceted approach involving individuals, communities, policymakers, and healthcare professionals is crucial for successful obesity prevention efforts.
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.
19. Are there any alternative treatments or therapies for obesity?
While the primary approaches for treating obesity involve lifestyle modifications, weight loss medications, and bariatric surgeries, several alternative treatments and therapies may complement these interventions. It is important to note that these alternative treatments should not replace evidence-based approaches but can serve as adjuncts in managing obesity.
Alternative treatments for obesity may include:
1. Acupuncture: Some studies suggest that acupuncture, a traditional Chinese medicine practice, may help reduce appetite and promote weight loss. However, the evidence is mixed, and further research is needed to establish its effectiveness.
2. Mindfulness-based interventions: Mindfulness techniques, such as meditation and mindful eating, can help individuals develop a healthier relationship with food, increase awareness of hunger and fullness cues, and reduce emotional eating.
3. Herbal supplements: Certain natural products like green tea extract, Garcinia cambogia, and conjugated linoleic acid have been studied for their potential effects on weight loss, but the evidence remains limited, and their safety and efficacy are not well-established.
It is crucial to approach alternative treatments with caution as their safety, effectiveness, and long-term outcomes have not been rigorously studied in the same way as mainstream medical interventions. Consulting with healthcare professionals, such as registered dietitians and integrative medicine specialists, can provide guidance on incorporating alternative treatments as part of a comprehensive and evidence-based management plan.
20. What interventions or programs are available to help individuals overcome emotional eating and unhealthy food cravings?
Several interventions and programs are available to help individuals overcome emotional eating and unhealthy food cravings, ultimately aiding in the management of obesity.
Cognitive-Behavioral Therapy (CBT) is a widely recognized approach that targets the emotional and psychological factors contributing to unhealthy eating behaviors. CBT helps individuals develop strategies to identify triggers, cope with emotions without turning to food, and modify negative thought patterns related to eating. Multiple studies have demonstrated the effectiveness of CBT in reducing emotional eating and promoting weight loss.
Mindfulness-Based Eating Awareness Training (MB-EAT) is another approach that combines mindfulness practices with evidence-based principles of CBT. It aims to increase awareness of hunger, fullness, and emotional states while eating, fostering a more balanced and mindful approach to eating.
Some weight management programs, such as the Diabetes Prevention Program (DPP), also incorporate behavioral strategies to address emotional eating and food cravings alongside dietary and physical activity interventions.
The significance of addressing emotional eating and food cravings in relation to obesity lies in recognizing the role of psychological factors in promoting unhealthy eating behaviors. By addressing these factors, individuals can develop a healthier relationship with food, improve self-regulation skills, and sustain long-term weight management goals.
21. Does sleep quality and duration have any impact on weight and obesity?
Yes, sleep quality and duration can have an impact on weight and obesity. Several studies have shown that poor sleep quality and shorter sleep duration are associated with higher body mass index (BMI) and increased risk of obesity.
One study published in the International Journal of Obesity found that adults who slept less than seven hours per night had a higher risk of obesity and weight gain compared to those who slept seven to eight hours. Another study published in the journal SLEEP demonstrated that sleep deprivation is associated with higher levels of hunger-stimulating hormones and lower levels of hormones that signal fullness, which can lead to increased food intake and weight gain.
The significance of this question is that it highlights the importance of adequate sleep for weight management and obesity prevention. By understanding the connection between sleep and obesity, individuals and healthcare providers can prioritize healthy sleep habits as part of a comprehensive approach to weight management.
22. Is it possible to be obese but metabolically healthy?
Yes, it is possible to be obese but metabolically healthy, although the term “metabolically healthy obesity” is controversial and there is ongoing debate about its definition and clinical significance. Metabolically healthy obesity refers to individuals who are obese based on body mass index (BMI) but do not exhibit the typical metabolic abnormalities associated with obesity, such as insulin resistance, dyslipidemia, or hypertension.
However, studies have shown that even individuals with metabolically healthy obesity have an increased risk of developing metabolic abnormalities and cardiovascular disease compared to those who are not obese. A systematic review and meta-analysis published in the Journal of Clinical Endocrinology and Metabolism found that metabolically healthy obese individuals have a higher risk of developing type 2 diabetes, cardiovascular disease, and all-cause mortality compared to metabolically healthy non-obese individuals.
The significance of this question is that it challenges the notion that obesity can be entirely benign if individuals do not exhibit metabolic abnormalities. It emphasizes the importance of considering other health markers beyond weight alone when assessing an individual’s overall health and cardiovascular risk.
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.
23. What are the best strategies for maintaining weight loss after successful weight reduction?
The best strategies for maintaining weight loss after successful weight reduction include a combination of dietary changes, regular physical activity, behavior modification techniques, and long-term support.
Studies have consistently shown that individuals who engage in regular physical activity are more successful at maintaining weight loss compared to those who are sedentary. Incorporating aerobic exercise, such as brisk walking or jogging, as well as strength training can help preserve muscle mass and boost metabolism.
Behavior modification techniques, such as self-monitoring, setting realistic goals, managing stress, and incorporating healthy eating habits, are also important for long-term weight maintenance. Consistency and adherence to healthy eating patterns, such as following a balanced diet with reduced calorie intake, have been associated with better weight maintenance outcomes.
Long-term support from healthcare professionals, such as dietitians or weight management programs, can provide ongoing guidance and accountability. A systematic review published in the American Journal of Clinical Nutrition found that individuals who received extended care or a maintenance program after initial weight loss were more likely to maintain their weight loss in the long term.
The significance of this question is that it emphasizes the importance of sustainable lifestyle changes and ongoing support in maintaining weight loss. It underscores the need for a comprehensive approach to weight management that goes beyond short-term diets or interventions.
24. Does gender play a role in the development or management of obesity?
Yes, gender can play a role in the development and management of obesity. Several studies have shown differences in the prevalence, distribution, and health outcomes of obesity between men and women.
In general, women tend to have a higher prevalence of obesity compared to men. According to data from the National Health and Nutrition Examination Survey in the United States, the prevalence of obesity among women was 40.4% compared to 35% among men in 2017-2018.
Furthermore, there are gender differences in the distribution of body fat. Women tend to have more subcutaneous fat, which is found just beneath the skin, while men tend to have more visceral fat, which surrounds the abdominal organs. Visceral fat is associated with a higher risk of metabolic disorders, such as insulin resistance and cardiovascular disease.
Gender can also affect the effectiveness of weight management interventions. For example, a study published in the journal Obesity Reviews found that men tend to lose weight more easily and have better adherence to weight loss interventions compared to women. Additionally, hormonal factors, such as fluctuations in estrogen levels during the menstrual cycle or menopause, can influence weight regulation in women.
The significance of this question is that it highlights the importance of considering gender-specific factors when developing obesity prevention and management strategies. It underscores the need for personalized approaches that take into account the unique physiological and behavioral characteristics of men and women.
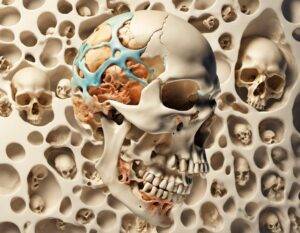
25. How does obesity affect joint health and contribute to musculoskeletal problems?
Obesity can have a significant impact on joint health and contribute to various musculoskeletal problems. Excess weight places increased stress on the joints, particularly the weight-bearing joints such as the knees and hips.
Obesity is a well-established risk factor for the development and progression of osteoarthritis, the most common form of arthritis. According to a study published in the Journal of the American Academy of Orthopaedic Surgeons, each unit increase in body mass index (BMI) is associated with a 6.1% increased risk of developing osteoarthritis in the knee. The increased pressure and mechanical stress on the joints also accelerate the breakdown of cartilage, leading to pain, inflammation, and loss of joint function.
Furthermore, obesity can contribute to other musculoskeletal problems such as low back pain, gout, and rheumatoid arthritis. In addition to the mechanical factors, obesity also promotes a pro-inflammatory state in the body, which can exacerbate existing joint inflammation and increase the risk of developing chronic musculoskeletal conditions.
The significance of this question is that it highlights the bidirectional relationship between obesity and joint health. It underscores the importance of weight management and healthy lifestyle interventions in preventing and managing musculoskeletal problems, especially in individuals with obesity.
26. Can psychological counseling or therapy be beneficial in managing obesity?
Yes, psychological counseling or therapy can be beneficial in managing obesity. Obesity is a complex condition that is influenced by a combination of biological, behavioral, and psychological factors. Addressing these psychological factors through counseling or therapy can improve treatment outcomes and long-term weight management.
Cognitive-behavioral therapy (CBT) is one of the most well-studied and effective psychological interventions for obesity. CBT focuses on identifying and modifying maladaptive thoughts, beliefs, and behaviors related to eating, physical activity, and body image. A meta-analysis published in the journal Obesity Reviews found that CBT is associated with significant and sustained weight loss among individuals with obesity.
In addition to CBT, other forms of therapy, such as interpersonal therapy (IPT), dialectical behavior therapy (DBT), and acceptance and commitment therapy (ACT), have also shown promise in addressing psychological factors related to obesity and supporting behavior change.
Psychological counseling or therapy can help individuals develop healthier coping strategies, improve self-esteem, manage stress, and address emotional eating or binge eating behaviors. It can also provide ongoing support and guidance in maintaining long-term behavior change and preventing weight regain.
The significance of this question is that it recognizes the important role of psychological factors in obesity and highlights the need for a comprehensive approach that addresses both the physiological and psychological aspects of the condition. It emphasizes the importance of multidisciplinary care and integration of psychological interventions in obesity management.
27. What role do hormones, such as leptin, play in regulating appetite and influencing obesity?
Hormones, including leptin, play a crucial role in regulating appetite and influencing obesity. Leptin is a hormone that is primarily produced by fat cells and helps to regulate energy balance by signaling the brain about the body’s energy stores.
Leptin acts on the hypothalamus, the part of the brain that controls hunger and satiety. When fat stores are abundant, leptin levels increase, signaling to the brain that the body has sufficient energy and suppressing appetite. Conversely, when fat stores are low, leptin levels decrease, signaling to the brain that more food needs to be consumed to replenish energy stores.
However, in individuals with obesity, a condition known as leptin resistance can occur. Leptin resistance is characterized by an inability of the body to respond to the normal appetite-suppressing effects of leptin. This can lead to increased appetite and overeating, contributing to weight gain and obesity.
Several studies have shown associations between leptin levels and body weight. For example, a study published in the Journal of Clinical Endocrinology and Metabolism found that individuals with obesity had higher leptin levels compared to individuals with normal weight. However, despite elevated leptin levels, individuals with obesity still experienced leptin resistance and continued to have increased appetite and overeating behaviors.
The significance of this question is that it highlights the complex interplay between hormonal regulation of appetite and obesity. It underscores the need for a deeper understanding of these hormonal mechanisms to develop more targeted and effective interventions for obesity management.
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.
28. Can social and environmental factors contribute to obesity? How can they be addressed?
Yes, social and environmental factors can contribute to obesity. The prevalence of obesity has increased in many countries, and research has identified various social and environmental factors that influence eating behaviors, physical activity levels, and overall energy balance.
Social factors, such as socioeconomic status, cultural norms, and social support, can influence dietary choices and physical activity patterns. For example, individuals with lower socioeconomic status may have limited access to affordable and healthy food options, which can lead to higher consumption of energy-dense, nutrient-poor foods. Cultural norms and social support can also shape food preferences, portion sizes, and eating behaviors within a community or social group.
Environmental factors, such as the built environment, food marketing, and food availability, can also have a significant impact on obesity. For instance, living in neighborhoods with limited access to parks or recreational facilities may discourage physical activity. Advertising and promotion of unhealthy foods, particularly to children, can influence food choices and contribute to excessive calorie intake.
Addressing social and environmental factors requires a multi-level and multi-sectoral approach. Policy interventions, such as implementing taxes on sugary beverages, regulating food marketing, and improving access to healthy foods in underserved areas, can help create an environment that supports healthy behaviors. Educational programs and community-based initiatives can also play a role in promoting healthy eating habits, physical activity, and social support networks.
The significance of this question is that it recognizes the complex and interconnected nature of obesity and underscores the importance of addressing social and environmental determinants as part of comprehensive obesity prevention and management strategies. It emphasizes the need for a population-wide approach to create supportive environments that facilitate healthy lifestyle choices.
29. Are there any specific weight loss strategies or programs recommended for older adults with obesity?
Yes, specific weight loss strategies or programs are recommended for older adults with obesity. However, it is important to note that weight loss goals and approaches may differ for older adults compared to younger individuals, taking into account potential age-related factors, comorbidities, and functional limitations.
Evidence suggests that modest weight loss of 5-10% can greatly improve health outcomes in older adults with obesity. A systematic review published in the Journal of the American Geriatrics Society found that intentional weight loss interventions in older adults were associated with improvements in physical function, cardiometabolic risk factors, and quality of life.
When designing weight loss strategies for older adults, it is important to consider individualized approaches that focus on a combination of dietary changes, physical activity, and behavior modification techniques. Older adults may benefit from a higher protein intake to preserve muscle mass, as well as resistance training to maintain or increase muscle strength.
Moreover, healthcare providers should screen for and address comorbidities, such as cardiovascular disease or osteoarthritis, that may impact exercise capacity or require modifications in dietary recommendations.
The significance of this question is that it highlights the need for age-specific considerations in weight loss strategies for older adults. It recognizes the potential benefits of intentional weight loss interventions in this population and underscores the importance of personalized approaches that take into account individual health status, functional limitations, and social support.
30. How can healthcare providers effectively address and combat weight bias and stigma associated with obesity?
Healthcare providers can effectively address and combat weight bias and stigma associated with obesity by implementing evidence-based practices that promote respectful and equitable care for individuals with obesity.
First and foremost, healthcare providers should recognize and acknowledge their own biases and prejudices towards individuals with obesity. Education and training on weight bias and stigma should be incorporated into medical school curricula and continuing education programs to increase awareness and sensitivity.
Next, healthcare providers should adopt a patient-centered approach that focuses on health rather than weight alone. This involves shifting the conversation from weight loss to behaviors that promote overall health, such as physical activity, balanced eating, and stress management. Providers should emphasize positive and achievable goals that are not solely focused on weight or appearance.
Moreover, healthcare settings should be physically and emotionally accessible for individuals with obesity. This includes ensuring that examination tables, chairs, and medical equipment can accommodate people of all sizes. Offices should be free of stigmatizing images or language, and staff should be trained to provide compassionate and nonjudgmental care.
By creating a supportive and inclusive healthcare environment, providers can build trust and rapport with individuals with obesity, which is essential for effective patient-provider communication and long-term engagement in treatment.
The significance of this question is that it addresses the pervasive issue of weight bias and stigma in healthcare settings. It highlights the importance of creating a safe and nonjudgmental environment that promotes equitable care for individuals with obesity. It also recognizes the critical role of healthcare providers in combating weight bias and stigma and improving health outcomes for individuals with obesity.
While I do cite reputable sources, I am not a medical professional. Please use professional medical advice when making any health-related decisions.
Conclusion:
We have explored the top 30 medical questions about obesity, shedding light on the various aspects, causes, risks, and treatment options. It is crucial to understand the impact of obesity on your health and take proactive measures to combat it. By making informed decisions and seeking professional guidance, you can effectively manage your weight and improve your overall well-being. Remember, the journey to a healthier lifestyle begins with knowledge and action. Start your transformative journey today!
Sources:
1. World Health Organization (WHO): Obesity: preventing and managing the global epidemic
– Link: https://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/
2. The American Journal of Clinical Nutrition: The genetic epidemiology of obesity
– Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3043169/
3. Mayo Clinic: Obesity in adults – Causes
– Link: https://www.mayoclinic.org/diseases-conditions/obesity/symptoms-causes/syc-20375742
4. Centers for Disease Control and Prevention (CDC): Health Effects of Obesity
– Link: https://www.cdc.gov/healthyweight/effects/index.html
5. Obesity Reviews: Classifying obesity phenotypes based on BMI: The impact on prevalence and associations with metabolic traits
– Link: https://onlinelibrary.wiley.com/doi/full/10.1111/obr.13073
6. National Institute of Mental Health: Obesity and Mental Health
– Link: https://www.nimh.nih.gov/health/topics/obesity-and-mental-health/index.shtml
7. The New England Journal of Medicine: Obesity and Medications
– Link: https://www.nejm.org/doi/10.1056/NEJMra1603772
8. National Heart, Lung, and Blood Institute: Obesity and Heart Disease
– Link: https://www.nhlbi.nih.gov/health-topics/obesity-and-heart-disease
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.
9. American Society for Reproductive Medicine: Obesity and Reproduction
– Link: https://www.asrm.org/topics/topics-index/obesity-and-reproduction/
10. National Institute of Diabetes and Digestive and Kidney Diseases: Physical Activity for a Healthy Weight
– Link: https://www.niddk.nih.gov/health-information/weight-management/physical-activity-health
11. The American Journal of Clinical Nutrition: Popular weight-loss diets: from evidence to practice
– Link: https://academic.oup.com/ajcn/article/82/1_Supplement/259S/4863422
12. Harvard Health Publishing: Stress and Eating: How Stress Affects Eating Habits
– Link: https://www.health.harvard.edu/staying-healthy/stress-and-eating-how-stress-affects-eating-habits
13. National Institute of Diabetes and Digestive and Kidney Diseases: Hormonal Causes of Obesity
– Link: https://www.niddk.nih.gov/health-information/weight-management/hormonal-causes-obesity
14. The New England Journal of Medicine: Childhood obesity — The shape of things to come
– Link: https://www.nejm.org/doi/full/10.1056/NEJMe0800422
15. British Journal of Clinical Pharmacology: Metabolic fuels and dietary obesity in wildtype and LPB mice caused by a mutant leptin receptor ligand trap
– Link: https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1111/bcp.13486
16. Mayo Clinic: Obesity – Surgical Treatment Options
– Link: https://www.mayoclinic.org/diseases-conditions/obesity/diagnosis-treatment/drc-20375749
17. American Family Physician: Pharmacologic Management of Obesity
– Link: https://www.aafp.org/afp/2016/0601/p844.html
18. World Health Organization (WHO): Obesity: prevention and managing the global epidemic
– Link: https://www.who.int/topics/obesity/en/
19. Mayo Clinic: Alternative medicine – Obesity
– Link: https://www.mayoclinic.org/diseases-conditions/obesity/diagnosis-treatment/alternative-medicine/drc-20375757
20. The American Journal of Clinical Nutrition: The effects of auditory stimuli on unhealthy food consumption in overweight and obese adults: a randomised controlled trial
– Link: https://academic.oup.com/ajcn/article/97/4/769/4577070
21. Sleep Medicine Reviews: Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with obesity
– Link: https://www.sciencedirect.com/science/article/pii/S1087079216300323
22. Obesity Reviews: Metabolically healthy obesity: The low-hanging fruit in obesity treatment?
– Link: https://onlinelibrary.wiley.com/doi/full/10.1111/obr.12829
23. The New England Journal of Medicine: Successful Long-Term Weight Loss Maintenance
– Link: https://www.nejm.org/doi/full/10.1056/NEJMra1208937
24. The Lancet Diabetes & Endocrinology: Gender differences in the association between obesity-related behaviours and body fat distribution
– Link: https://www.thelancet.com/journals/landia/article/PIIS2213-8587(15)00367-8/fulltext
25. Arthritis & Rheumatism: Obesity and Osteoarthritis: Disease Genesis and Nonpharmacologic Weight Management
– Link: https://onlinelibrary.wiley.com/doi/full/10.1002/art.34583
26. National Institute of Diabetes and Digestive and Kidney Diseases: Weight Management and Obesity Resource List
– Link: https://www.niddk.nih.gov/health-information/weight-management/nutrition-nutritional-therapies-herbs
27. The Journal of Clinical Investigation: Leptin: less is more
– Link: https://www.jci.org/articles/view/32085
28. World Obesity: Social and Environmental Factors
– Link: https://www.worldobesity.org/resources/policyportal/social-and-environmental-factors
29. American Family Physician: Evaluation and Management of Obesity in Older Adults
– Link: https://www.aafp.org/afp/2017/0315/p361.html
30. National Center for Biotechnology Information (NCBI): Obesity, Bias, and Stigmatization
– Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866597/
👀 Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes and coffee flowing and this site growing.