The Silent Threat: Unveiling the Hidden Dangers
of
Osteoporosis
Unlocking the Secrets of Osteoporosis: Your Definitive Guide to Understanding and Treating this Silent Bone Disease. Discover expert-backed answers to the top 40 questions that demystify osteoporosis, offering invaluable insights and empowering you to take charge of your bone health. Dive into this comprehensive report and uncover the knowledge you need to build strong, resilient bones for a lifetime.
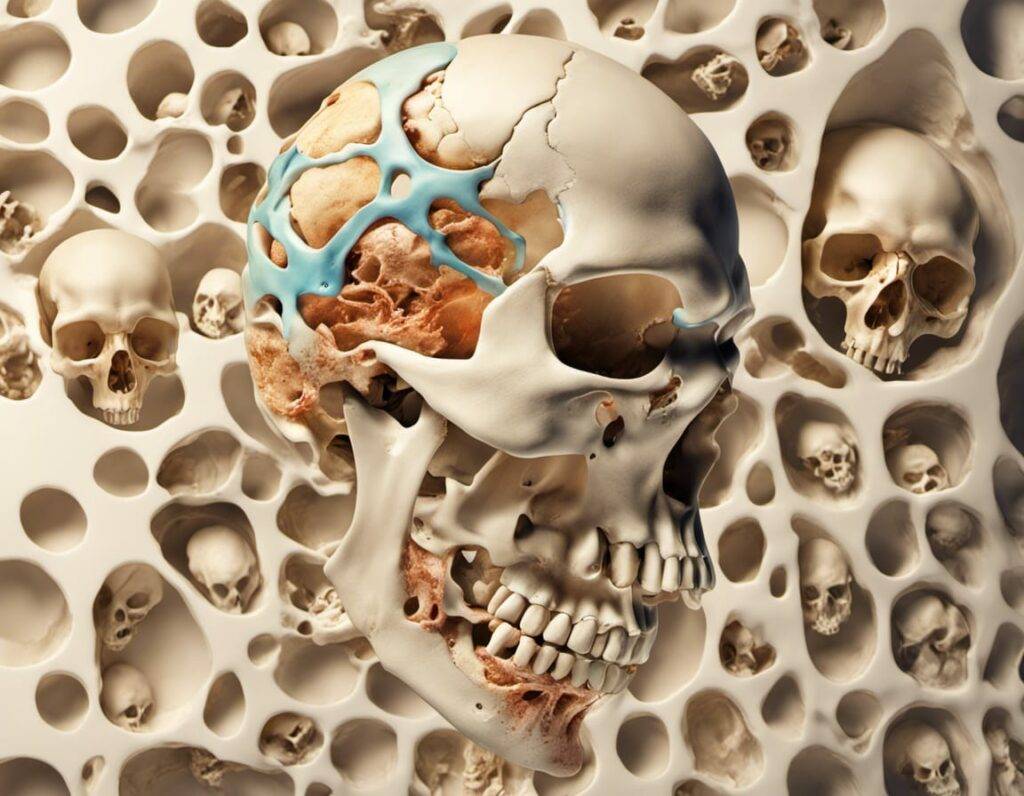
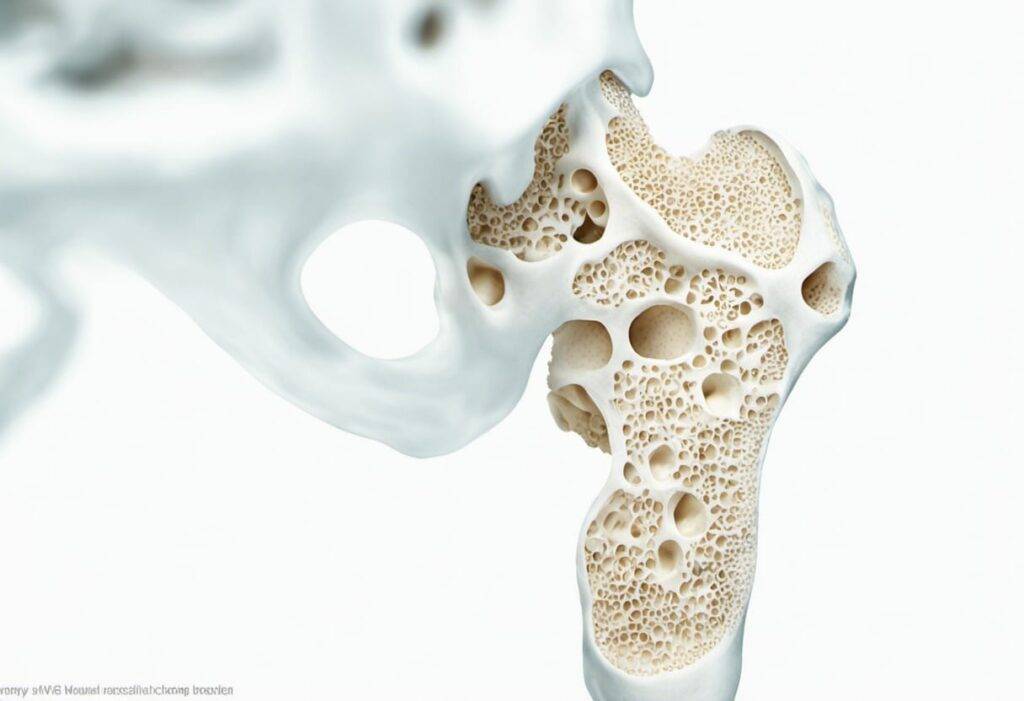
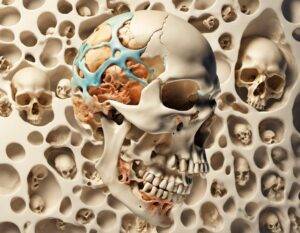
1. What is osteoporosis and how does it affect the bones?
Osteoporosis is a progressive bone disease characterized by low bone density and deterioration of bone tissue, leading to brittle and fragile bones. It occurs when the body loses too much bone, makes too little bone, or both. As a result, the bones become weak and can easily fracture or break even with minor falls or bumps [National Osteoporosis Foundation. (n.d.). About Osteoporosis. Retrieved from https://www.nof.org/preventing-fractures/general-facts/what-women-need-to-know-about-osteoporosis/]. Osteoporosis primarily affects the spine, hips, and wrists, but can also impact other bones in the body [Mayo Clinic Staff. (2021, April20). Osteoporosis. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968].
2. What are the main causes of osteoporosis?
Osteoporosis can be caused by various factors, including:
– Aging: As people age, their bones naturally become less dense and weaker, increasing the risk of osteoporosis.
– Hormonal changes: Reduced estrogen levels in women during menopause and reduced testosterone levels in men can contribute to bone loss.
– Lack of calcium and vitamin D: Inadequate intake of calcium and vitamin D, essential nutrients for maintaining bone health, can increase the risk of osteoporosis.
– Sedentary lifestyle: Lack of regular exercise and physical activity can lead to bone loss and weakened bones.
– Long-term use of certain medications: Prolonged use of corticosteroids, anticonvulsants, and some cancer treatments can increase the risk of osteoporosis.
– Medical conditions: Certain medical conditions, such as rheumatoid arthritis, celiac disease, and hormonal disorders, can contribute to bone loss.
Reference:
National Osteoporosis Foundation. (n.d.). Risk Factors. Retrieved from https://www.nof.org/preventing-fractures/general-facts/risk-factors/
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
3. What are the primary risk factors for developing osteoporosis?
Several risk factors increase the likelihood of developing osteoporosis, including:
– Age: The risk of osteoporosis increases with age, as bone density tends to decrease over time.
– Gender: Women are more prone to osteoporosis than men, especially after menopause, due to a rapid decline in estrogen levels.
– Family history: Having a parent or sibling with osteoporosis increases the likelihood of developing the condition.
– Body size: Individuals with a small body frame or low body weight have a higher risk of osteoporosis.
– Hormonal changes: Disorders affecting hormone levels, such as early menopause or low testosterone, can contribute to bone loss.
– Nutritional deficiencies: Low intake of calcium, vitamin D, and other essential nutrients can weaken bones and increase the risk of osteoporosis.
– Sedentary lifestyle: Lack of exercise and physical activity weakens bones and increases the risk of osteoporosis.
Reference:
Mayo Clinic Staff. (2021, April20). Osteoporosis. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
4. Are there any genetic factors that influence the development of osteoporosis?
Yes, genetics can play a role in the development of osteoporosis. Research suggests that individuals with a family history of osteoporosis have a higher risk of developing the condition. Specific genes related to bone metabolism and mineral density have been identified as potential contributors to the development of osteoporosis [National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2017, June). Osteoporosis. Retrieved from https://www.niams.nih.gov/health-topics/osteoporosis#tab-overview]. However, it is important to note that genetics alone do not determine whether a person will develop osteoporosis. Environmental and lifestyle factors also significantly influence the risk.
5. How does age impact the risk of developing osteoporosis?
Age is a significant risk factor for developing osteoporosis. As people get older, their bones naturally become less dense and weaker, making them more susceptible to fractures and breaks. Bone loss typically accelerates after menopause in women due to a decrease in estrogen levels, resulting in faster bone deterioration. In men, testosterone levels decline gradually with age, which can also contribute to bone loss. It is crucial to prioritize bone health through proper nutrition, regular exercise, and preventive measures as age increases to minimize the risk of osteoporosis.
Reference:
National Osteoporosis Foundation. (n.d.). Commonly Asked Questions. Retrieved from https://www.nof.org/patients/fracturesfall-prevention/preventing-falls-and-related-fractures/adults-at-risk/osteoporosis-faqs/
6. Can hormonal changes, such as menopause, increase the risk of osteoporosis?
Yes, hormonal changes, particularly during menopause, can increase the risk of osteoporosis. Estrogen plays a crucial role in maintaining bone density, and as women enter menopause, their estrogen levels decline. This decline in estrogen can accelerate bone loss and lead to osteoporosis. It is estimated that women can lose up to20% of their bone density in the five to seven years following menopause. Additionally, other hormonal imbalances or conditions that cause hormonal changes can also increase the risk of osteoporosis.
Reference: American College of Obstetricians and Gynecologists. (2017). Osteoporosis. Retrieved from https://www.acog.org/womens-health/faqs/osteoporosis
7. What role does calcium play in bone health and preventing osteoporosis?
Calcium is essential for maintaining strong and healthy bones, as well as preventing osteoporosis. Our bodies continually remove and replace calcium from our bones in a process called remodeling. If we don’t consume enough calcium-rich foods or if our bodies have difficulty absorbing calcium, our bones can become weak and brittle. Adequate calcium intake throughout life, especially during childhood and adolescence when bones are still developing, helps to maximize bone density.
Reference: National Osteoporosis Foundation. (2021). Calcium and Vitamin D: What You Need to Know. Retrieved from https://www.nof.org/patients/treatment/calciumvitamin-d/
8. How does a lack of vitamin D affect bone health and contribute to osteoporosis?
Vitamin D is crucial for proper bone health, as it helps the body absorb calcium from the digestive system. Without sufficient vitamin D, even if you consume an adequate amount of calcium, your body won’t be able to utilize it effectively. A lack of vitamin D can lead to decreased calcium absorption, causing decreased bone density and an increased risk of osteoporosis.
Reference: Mayo Clinic. (2021). Calcium and vitamin D: Important at every age. Retrieved from https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/calcium-supplements/faq-20058238
9. What lifestyle factors can increase the risk of developing osteoporosis?
Several lifestyle factors can increase the risk of developing osteoporosis:
– Sedentary lifestyle: Lack of weight-bearing exercises, such as walking or weightlifting, can contribute to bone loss and increase the risk of osteoporosis.
– Smoking: Smoking negatively affects bone health and increases the risk of fractures.
– Excessive alcohol consumption: Consuming more than moderate amounts of alcohol can weaken bones and increase the risk of osteoporosis.
– Poor nutrition: Inadequate intake of calcium, vitamin D, and other essential nutrients can lead to weaker bones and higher osteoporosis risk.
Reference: International Osteoporosis Foundation. (n.d.). Lifestyle Risk Factors. Retrieved from https://www.iofbonehealth.org/facts-statistics/lifestyle-risk-factors
10. Are there any medications or medical conditions that can contribute to osteoporosis?
Yes, certain medications and medical conditions can contribute to the development of osteoporosis. Some medications known to increase the risk of bone loss and osteoporosis include long-term use of corticosteroids (such as prednisone), selective serotonin reuptake inhibitors (SSRIs), certain anticonvulsants, and aromatase inhibitors. Furthermore, medical conditions such as rheumatoid arthritis, celiac disease, inflammatory bowel disease, hyperthyroidism, and certain hormonal disorders can also contribute to osteoporosis.
Reference: National Osteoporosis Foundation. (2021). Medications That Can Cause Bone Loss, Falls and/or Fractures. Retrieved from https://www.nof.org/patients/treatment/medicationadherence/medications-that-can-causebone-loss-falls-andor-fractures
11. What are the early signs and symptoms of osteoporosis?
Early signs and symptoms of osteoporosis may not be apparent until a fracture occurs. However, some individuals may experience:
a) Back pain: Persistent and dull back pain, caused by fractures or collapsed vertebrae.
b) Loss of height: Gradual loss of height over time due to weakened vertebrae.
c) Stooped posture: The weakening of the spine can lead to a hunched or stooped posture.
d) Receding gums: Osteoporosis can affect the jawbone, leading to gum recession and tooth loss.
e) Weakened grip strength: Osteoporosis-related fractures in the wrist or hand can result in decreased grip strength.
Reference: Mayo Clinic. Understanding Osteoporosis – Symptoms & Causes. (https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968)
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
12. How does osteoporosis progress and what are the potential complications?
Osteoporosis is a progressive condition that weakens bones and increases the risk of fractures. It typically progresses silently without noticeable symptoms until a fracture occurs. Complications of osteoporosis may include:
a) Fractures: The most common complication, particularly in the wrist, spine, and hip, resulting in pain, disability, and loss of independence.
b) Loss of mobility: Fractures may lead to restricted mobility, making daily activities challenging.
c) Chronic pain: Vertebral fractures can cause chronic pain and difficulty in performing daily tasks.
d) Spinal deformity: Multiple vertebral fractures can cause the spine to curve, leading to a hunchback appearance (kyphosis).
Reference: National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. (https://cdn.nof.org/wp-content/uploads/2016/09/Clinicians-Guide-to-Prevention-and-Treatment-of-Osteoporosis.pdf)
13. What are the most reliable diagnostic methods for osteoporosis?
The most reliable diagnostic methods for osteoporosis include:
a) Dual-energy X-ray absorptiometry (DXA): This is the preferred method for measuring bone mineral density (BMD) and assessing fracture risk. DXA scans are commonly performed on the hip and spine, providing T-scores that compare bone density to the average peak bone density of young, healthy adults.
b) FRAX tool: The Fracture Risk Assessment Tool calculates the 10-year probability of hip and major osteoporotic fractures, considering clinical risk factors along with BMD measurements if available.
Reference: National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. (https://cdn.nof.org/wp-content/uploads/2016/09/Clinicians-Guide-to-Prevention-and-Treatment-of-Osteoporosis.pdf)
14. What tests are used to measure bone density and assess the risk of fractures?
Tests used to measure bone density and assess the risk of fractures include:
a) Dual-energy X-ray absorptiometry (DXA): DXA scans are the gold standard for measuring bone density and determining fracture risk. They measure the mineral content, such as calcium, in specific bones.
b) Quantitative ultrasound (QUS): QUS assesses bone density using sound waves, typically measuring the heel.
c) Computed tomography (CT) scan: Although not routinely used, CT scans can provide precise measurements of bone density.
Reference: National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. (https://cdn.nof.org/wp-content/uploads/2016/09/Clinicians-Guide-to-Prevention-and-Treatment-of-Osteoporosis.pdf)
15. Are there any specific imaging techniques used to diagnose osteoporosis?
Yes, specific imaging techniques can be used to diagnose osteoporosis, such as:
a) X-rays: While not capable of measuring bone density accurately, X-rays can detect fractures and evaluate bone structure.
b) Magnetic resonance imaging (MRI): MRI can detect fractures, assess bone quality, and identify early signs of osteoporosis before bone density loss is significant.
c) Quantitative computed tomography (QCT): QCT is a specialized CT scan that provides three-dimensional measurements of bone density in specific areas. It is more accurate than DXA in assessing the spine.
Reference: National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. (https://cdn.nof.org/wp-content/uploads/2016/09/Clinicians-Guide-to-Prevention-and-Treatment-of-Osteoporosis.pdf)
16. What are the recommended dietary modifications for individuals at risk of osteoporosis?
To maintain and improve bone health, individuals at risk of osteoporosis should consider the following dietary modifications:
a. Calcium intake: It is recommended to consume an adequate amount of calcium daily, which is around1000-1200 mg for most adults[National Institutes of Health, Office of Dietary Supplements. Calcium – Health Professional Fact Sheet. (https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/)]. Good sources of calcium include dairy products like milk, cheese, and yogurt, as well as fortified plant-based milk, leafy greens like broccoli and kale, and calcium-fortified foods.
b. Vitamin D consumption: Vitamin D helps the body absorb calcium efficiently. The recommended daily intake of vitamin D is around600-800 IU (International Units)[National Institutes of Health, Office of Dietary Supplements. Vitamin D – Health Professional Fact Sheet. (https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/)]. Sources of vitamin D include fatty fish like salmon and mackerel, fortified dairy products, egg yolks, and sunlight exposure.
c. Protein intake: Consuming an adequate amount of protein is crucial for maintaining bone health as it helps in building and repairing bone tissue[National Osteoporosis Foundation. Protein and Bone Health. (https://www.nof.org/patients/treatment/nutrition/)]. Good sources of protein include lean meats, poultry, fish, beans, legumes, and tofu.
d. Limiting alcohol and caffeine consumption: Excessive alcohol intake and high caffeine consumption can negatively affect bone health and increase the risk of osteoporosis. It is advisable to limit alcohol to moderate levels (up to one drink per day for women and up to two drinks per day for men) and reduce caffeine intake.
e. Avoiding smoking: Smoking has been linked to decreased bone density and an increased risk of fractures. Quitting smoking or avoiding it altogether is essential for maintaining optimal bone health[National Institute of Arthritis and Musculoskeletal and Skin Diseases. Smoking and Bone Health. (https://www.bones.nih.gov/health-info/bone/osteoporosis/conditions-behaviors/bone-smoking].
17. Can nutritional supplements slow down the progression or prevent osteoporosis?
Nutritional supplements can play a role in slowing down the progression or helping to prevent osteoporosis in certain individuals. However, it is important to note that supplements should not replace a healthy diet.
a. Calcium supplements: If individuals are unable to consume enough calcium through their diet, calcium supplements may be recommended. It is important to choose calcium citrate or calcium carbonate supplements with vitamin D for better absorption[National Institutes of Health, Office of Dietary Supplements. Calcium – Health Professional Fact Sheet. (https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/)].
b. Vitamin D supplements: For individuals with limited sun exposure, especially in regions with less sun during certain months, vitamin D supplements can help meet the daily recommended intake. The dosage should be discussed with a healthcare professional[National Institutes of Health, Office of Dietary Supplements. Vitamin D – Health Professional Fact Sheet. (https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/)].
c. Other supplements: There is limited evidence supporting the use of other supplements such as vitamin K, magnesium, or specific forms of collagen in preventing or slowing down osteoporosis. Further research is needed to establish their effectiveness.
It is crucial to consult with a healthcare professional before starting any supplements, as excessive intake of certain nutrients can have adverse effects.
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
18. How does exercise impact bone health and reduce the risk of osteoporosis?
Exercise plays a vital role in maintaining and improving bone health. Regular physical activity can help reduce the risk of osteoporosis in the following ways:
a. Strengthening bones: Weight-bearing exercises, such as walking, jogging, dancing, and resistance training, put stress on bones and stimulate bone remodeling. This process leads to increased bone density and overall strength[National Osteoporosis Foundation. Exercise for Strong Bones. (https://www.nof.org/patients/fracturesfall-prevention/exercisesafe-movement/exercise-for-strong-bones/)].
b. Improving balance and coordination: Certain exercises, such as tai chi and yoga, not only enhance muscle strength but also improve balance and coordination. This can help prevent falls, which are a significant cause of fractures in individuals with osteoporosis[Harvard Health Publishing. Strengthen Your Bones with Exercise. (https://www.health.harvard.edu/staying-healthy/strengthen-your-bones-with-exercise)].
c. Generating mechanical stress: Activities that involve impact or high-intensity exercises create mechanical stress on bones, which triggers the bone-forming cells to build stronger and more dense bones[Mayo Clinic. Exercise: A Bone Builder and Preserver. (https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/bone-health/art-20045060)].
d. Promoting muscle strength: Strong muscles help support and protect bones, reducing the risk of fractures. Resistance exercises, like weightlifting or using resistance bands, can enhance muscle mass and strength, further improving bone health[International Osteoporosis Foundation. Exercise. (https://www.iofbonehealth.org/exercise-0)].
e. Enhancing overall well-being: Regular exercise also contributes to maintaining a healthy body weight, improving cardiovascular health, and reducing the risk of other chronic conditions associated with osteoporosis, such as heart disease and type2 diabetes[National Osteoporosis Foundation. Osteoporosis Exercise: The Bone-Building Solution. (https://www.nof.org/patients/treatment/nutrition/)].
It is recommended to engage in a combination of weight-bearing, muscle-strengthening, and balance-enhancing exercises. Consulting with a healthcare professional or a qualified exercise specialist can help design an exercise regimen suitable for individual needs.
19. What types of exercises are most beneficial for individuals prone to osteoporosis?
Individuals prone to osteoporosis can benefit from incorporating the following types of exercises into their routine:
a. Weight-bearing exercises: Activities where you bear your body weight through your legs, such as walking, jogging, dancing, stair climbing, and hiking, are excellent for stimulating bone growth[National Osteoporosis Foundation. Exercise for Strong Bones. (https://www.nof.org/patients/fracturesfall-prevention/exercisesafe-movement/exercise-for-strong-bones/)]. These exercises place stress on the bones, helping to improve bone density and strength.
b. Strength training exercises: Resistance exercises, such as weightlifting, using resistance bands, or doing bodyweight exercises like push-ups and squats, can help build muscle strength, which in turn supports and protects bones[Harvard Health Publishing. Strengthen Your Bones with Exercise. (https://www.health.harvard.edu/staying-healthy/strengthen-your-bones-with-exercise)]. It is advisable to include exercises that target major muscle groups, such as the legs, hips, back, abdomen, chest, and arms.
c. Balance and coordination exercises: These exercises improve balance, stability, and reduce the risk of falls. Activities like tai chi, yoga, and specific balance exercises can enhance proprioception, coordination, and overall postural control[National Osteoporosis Foundation. Exercise and Physical Activity: What’s the Difference and How Much Do I Need? (https://www.nof.org/patients/fracturesfall-prevention/exercisesafe-movement/exercise-and-physical-activity-what-s-the-difference-and-how-much-do-i-need-/)].
d. Flexibility exercises: Stretching exercises like yoga or Pilates help improve flexibility, mobility, and maintain joint health. They also provide an opportunity to work on posture and balance, reducing the risk of falls and fractures[Brigham and Women’s Hospital. Exercise for Bone Health. (https://www.brighamandwomens.org/medicine/endocrinology/diseases-and-conditions/osteoporosis/for-healthcare-professionals/exercise-for-bone-health)].
Combining these different types of exercises into a well-rounded fitness routine can maximize the benefits for individuals prone to osteoporosis. It is important to consult with a healthcare professional or an exercise specialist to ensure exercises are performed correctly and safely.
20. Can hormone replacement therapy (HRT) be used to treat osteoporosis?
Hormone replacement therapy (HRT) can be used as a treatment option for osteoporosis in certain cases. HRT involves supplementing hormonal levels, mainly estrogen and progesterone, to compensate for the hormonal changes that occur during menopause. It helps slow down bone loss and reduce the risk of fractures. However, the decision to use HRT should be customized based on an individual’s overall health, medical history, and other factors. It is essential to consult with a healthcare professional to determine if HRT is suitable and safe, as it has both benefits and potential risks.
Reference:
National Osteoporosis Foundation. Hormone Therapy and Osteoporosis. (https://www.nof.org/patients/treatment/hormone-therapy/)
21. What medications are commonly prescribed to treat osteoporosis?
Commonly prescribed medications for the treatment of osteoporosis include bisphosphonates, selective estrogen receptor modulators (SERMs), calcitonin, and denosumab. Other medications such as teriparatide and romosozumab may also be prescribed in specific cases.
National Osteoporosis Foundation. (n.d.). Medications. Retrieved from https://www.nof.org/patients/treatment/medications/
22. Are there any potential side effects or risks associated with osteoporosis medications?
While osteoporosis medications can be effective in treating the condition, they may also have potential side effects and risks. Bisphosphonates, for example, can cause gastrointestinal side effects such as stomach upset and acid reflux. In rare cases, they may also lead to osteonecrosis of the jaw or atypical fractures. SERMs may increase the risk of blood clots, while calcitonin can cause nasal irritation and flushing. It is important to weigh the benefits and risks of these medications with your healthcare provider.
Mayo Clinic. (2021). Osteoporosis drugs: Safe use, side effects and interactions. Retrieved from https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/osteoporosis-drugs/art-20045070
23. How do bisphosphonates work and what should be considered while taking them?
Bisphosphonates work by inhibiting the activity of cells called osteoclasts, which are responsible for breaking down bone tissue. By reducing osteoclast activity, bisphosphonates help prevent further bone loss and increase bone density. It is important to take bisphosphonates as prescribed, usually on an empty stomach in the morning, and to remain upright for at least 30 minutes after taking the medication. This helps minimize the risk of side effects such as acid reflux and esophageal irritation.
National Osteoporosis Foundation. (n.d.). Bisphosphonates for Osteoporosis. Retrieved from https://www.nof.org/patients/treatment/medicationadherence/osteoporosis-medication-fact-sheet/
24. What are the possible benefits and risks of using calcitonin for osteoporosis treatment?
Calcitonin is a hormone that helps regulate calcium levels in the body. When used for osteoporosis treatment, calcitonin can help slow down bone loss. However, the benefits of calcitonin in terms of fracture prevention are modest compared to other medications. Additionally, calcitonin may cause nasal irritation and flushing. It is typically administered as a nasal spray or injection under the skin. If considering calcitonin for treatment, discuss the potential benefits and risks with your healthcare provider.
International Osteoporosis Foundation. (2020). Calcitonin fact sheet. Retrieved from https://www.iofbonehealth.org/calcitonin-fact-sheet
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
25. Can selective estrogen receptor modulators (SERMs) be used to prevent or treat osteoporosis?
Yes, selective estrogen receptor modulators (SERMs) can be used in the prevention and treatment of osteoporosis. SERMs work by binding to estrogen receptors and mimicking the effects of estrogen in some tissues, while blocking estrogen in others. This helps to preserve bone density and reduce the risk of fractures. However, it is important to note that SERMs may increase the risk of blood clots, and regular monitoring is necessary while taking these medications. Talk to your healthcare provider to determine if SERMs are an appropriate option for you.
MedlinePlus. (2021). SERMs: MedlinePlus Drug Information. Retrieved from https://medlineplus.gov/druginfo/meds/a699035.html
26. What role does parathyroid hormone (PTH) play in the treatment of osteoporosis?
Parathyroid hormone (PTH) is a hormone produced by the parathyroid glands that plays a crucial role in the regulation of calcium and phosphate levels in the body. In the treatment of osteoporosis, PTH is used in the form of a medication called teriparatide (Forteo).
Teriparatide works by increasing bone formation and promoting the differentiation of osteoblasts, the cells responsible for building new bone. It also enhances the absorption of dietary calcium and reduces the excretion of calcium in the urine. By stimulating bone remodeling, teriparatide helps to increase bone density and strength, reducing the risk of fractures in individuals with osteoporosis.
It is important to note that teriparatide is usually prescribed for individuals at high risk of fracture or who have not responded well to other osteoporosis medications. It is typically administered as a daily injection for a limited period, usually up to 2 years. Therefore, it is crucial to consult with a healthcare professional to determine the right treatment plan for each individual.
Reference:
National Osteoporosis Foundation. (2021). Osteoporosis: Treatment. Retrieved from https://www.nof.org/patients/treatment/osteoporosis-treatment/
27. Are there any alternative or complementary therapies that can help manage osteoporosis?
While alternative or complementary therapies should not be used as a replacement for conventional medical treatments, some individuals may find certain approaches helpful in managing osteoporosis. It is essential to keep in mind that evidence for the effectiveness of these therapies is often limited, and it is important to discuss them with a healthcare professional before initiating any new treatment.
Some alternative or complementary therapies that have been studied for their potential benefits in osteoporosis include:
1. Acupuncture: Some studies suggest that acupuncture may help reduce pain associated with osteoporotic fractures and improve quality of life in individuals with the condition.
2. Herbal remedies: Certain herbal supplements, such as red clover and black cohosh, have been explored for their potential in improving bone health. However, more research is needed to establish their efficacy and safety.
3. Yoga and Tai Chi: These mind-body exercises have been shown to improve balance, flexibility, and strength, which can help reduce the risk of falls and fractures among individuals with osteoporosis.
While these alternative therapies may offer some benefits, they should be used cautiously, and individuals should consult with their healthcare provider before incorporating them into their treatment plan.
Reference:
Osteoporosis Canada. (2021). Complementary and Alternative Therapies. Retrieved from https://osteoporosis.ca/living-with-osteoporosis/treatment/complementary-therapies/
28. What impact does smoking have on bone health and osteoporosis risk?
Smoking has a detrimental impact on bone health and significantly increases the risk of developing osteoporosis. Here are some key points to understand the relationship between smoking and osteoporosis:
1. Reduced bone density: Smoking is associated with lower bone mineral density, which is a key factor in the development of osteoporosis. Studies have shown that smokers have a higher risk of experiencing rapid bone loss and fractures compared to non-smokers.
2. Hormonal imbalances: Smoking can disrupt hormone production in the body, leading to an imbalance in estrogen levels, especially in women. Estrogen plays a crucial role in maintaining bone health, and a deficiency can accelerate bone loss.
3. Impaired calcium absorption: Smoking interferes with the body’s ability to absorb and utilize calcium effectively. Calcium is a vital mineral for bone health, and inadequate absorption can contribute to the development of osteoporosis.
4. Reduced blood supply to bones: Smoking damages blood vessels, leading to reduced blood supply to bones. This hampers the delivery of essential nutrients and oxygen to bone tissues, impairing their ability to regenerate and maintain strength.
5. Impaired bone healing: Smoking adversely affects the healing process of fractures. Smokers have a higher risk of delayed fracture healing, non-union, and postoperative complications.
Quitting smoking is crucial for preserving bone health and reducing the risk of osteoporosis. By quitting smoking, individuals can slow down bone loss, improve calcium absorption, and enhance overall bone strength.
Reference:
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2020). Osteoporosis: Frequently Asked Questions. Retrieved from https://www.niams.nih.gov/health-topics/osteoporosis#tab-overview
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
29. Does excessive alcohol consumption increase the risk of developing osteoporosis?
Excessive alcohol consumption can indeed increase the risk of developing osteoporosis. Here’s what you need to know about the relationship between alcohol and osteoporosis:
1. Negative impact on bone formation: Alcohol interferes with the body’s ability to absorb calcium, a crucial mineral for bone strength. It also inhibits the production of new bone tissue by suppressing osteoblasts, the cells responsible for bone formation.
2. Hormonal imbalances: Chronic alcohol use can disrupt hormone production and balance in the body. This can lead to reduced levels of estrogen, which plays a vital role in maintaining bone health in both men and women.
3. Increased risk of falls: Alcohol consumption impairs balance and coordination, increasing the risk of falls and fractures. Falls are a significant cause of fractures in individuals with osteoporosis.
4. Nutritional deficiencies: Alcohol abuse often leads to poor nutrition and vitamin deficiencies. Inadequate intake of calcium, vitamin D, and other essential nutrients further undermines bone health.
5. Liver dysfunction: Chronic alcohol consumption can damage the liver, affecting its ability to activate vitamin D, which is important for calcium absorption and bone health.
It is important to note that moderate alcohol consumption (up to one drink per day for women and up to two drinks per day for men) may not significantly increase the risk of osteoporosis. However, excessive and chronic alcohol use should be avoided to protect bone health.
Reference:
Mayo Clinic. (2020). Alcohol Use: If You Drink, Do So in Moderation. Retrieved from https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/alcohol/art-20044551
30. How does caffeine intake affect bone health and contribute to osteoporosis?
Caffeine intake can have some impact on bone health, but the effects are relatively minor compared to other risk factors for osteoporosis. Here’s what you should know:
1. Calcium excretion: Caffeine is a diuretic, meaning it increases urine production. Some studies suggest that consuming large amounts of caffeine (more than 400 mg per day, equivalent to about four cups of brewed coffee) may slightly increase calcium excretion through urine. However, this effect seems to be temporary and doesn’t significantly affect overall calcium balance in individuals with an adequate calcium intake.
2. Reduced calcium absorption: Caffeine may modestly reduce calcium absorption in the intestines. However, studies have shown that this effect can be counteracted by consuming calcium-rich foods or supplements along with caffeine.
3. Insufficient evidence for significant harm: While excessive caffeine intake may have some minor impact on calcium metabolism, current research does not support the claim that moderate caffeine consumption increases the risk of osteoporosis or fractures. Other lifestyle factors, such as inadequate physical activity, smoking, and low calcium intake, have a much greater impact on bone health.
It is important to maintain a balanced diet, including adequate calcium intake, to support healthy bones. If you consume caffeine, being mindful of your overall calcium intake and ensuring regular physical activity can help mitigate any potential effects on bone health.
Reference:
International Osteoporosis Foundation. (2021). Caffeine and Bone Health. Retrieved from https://www.osteoporosis.foundation/educational-hub/patient-courses/caffeine-and-bone-health
31. Can certain medical conditions, such as rheumatoid arthritis or celiac disease, increase the risk of osteoporosis?
Certain medical conditions can increase the risk of osteoporosis. For example, rheumatoid arthritis and celiac disease are two conditions that have been associated with an increased risk of osteoporosis. Rheumatoid arthritis is an autoimmune disease that causes inflammation in the joints, and this chronic inflammation can lead to bone loss over time. Celiac disease, on the other hand, is an autoimmune disorder characterized by an intolerance to gluten. People with celiac disease often have malabsorption issues that can result in nutrient deficiencies, including calcium and vitamin D, which are important for bone health.
Research has shown that individuals with rheumatoid arthritis are at an increased risk of developing osteoporosis due to the inflammatory process involved in the disease. In fact, the prevalence of osteoporosis in rheumatoid arthritis patients is significantly higher compared to the general population. Similarly, celiac disease can lead to osteoporosis because the body’s inability to properly absorb nutrients can affect bone strength and density.
It is important for individuals with these medical conditions to work closely with their healthcare providers to manage their symptoms and monitor their bone health. Regular screenings, such as bone density tests, may be recommended to assess the risk of osteoporosis and guide treatment decisions.
References:
– National Osteoporosis Foundation. (n.d.). Rheumatoid Arthritis and Osteoporosis. Retrieved from https://www.nof.org/patients/what-is-osteoporosis/causes/rheumatoid-arthritis/
– National Osteoporosis Foundation. (n.d.). Celiac Disease & Osteoporosis. Retrieved from https://www.nof.org/patients/fracturesfall-prevention/osteoporosis-and-celiac-disease/
32. Are there any surgical options available for severe cases of osteoporosis?
In severe cases of osteoporosis where fractures are frequent and significantly affecting quality of life, surgical options may be considered. These surgical interventions aim to stabilize fractures, relieve pain, and improve mobility for individuals with advanced osteoporosis.
One surgical option is vertebroplasty, which involves injecting a special cement-like material into fractured vertebrae. This procedure helps to stabilize the fractured bone and reduce pain. Another similar procedure is kyphoplasty, in which a balloon is first inserted into the fractured vertebrae and inflated to create a cavity. The cavity is then filled with the cement-like material to restore the height of the vertebrae and provide stabilization.
It is important to note that while these surgical options can help manage fractures and alleviate pain, they do not address the underlying bone loss in osteoporosis. Therefore, surgical interventions are typically used in combination with other treatments, such as medication, physical therapy, and lifestyle modifications, to manage osteoporosis as a whole.
References:
– Mayo Clinic. (2020). Vertebroplasty. Retrieved from https://www.mayoclinic.org/tests-procedures/vertebroplasty/about/pac-20385220
– University of Rochester Medical Center. (n.d.). Kyphoplasty. Retrieved from https://www.urmc.rochester.edu/orthopaedics/conditions-treatments/kyphoplasty.aspx
33. Can a healthy diet alone prevent or reverse osteoporosis?
While a healthy diet plays a crucial role in maintaining overall bone health, it is not sufficient alone to prevent or reverse osteoporosis. Osteoporosis is a complex condition influenced by various factors, including age, genetics, hormonal status, and lifestyle choices. Although nutrition is an essential component, it should be complemented by other preventive and treatment measures.
A well-balanced diet rich in calcium and vitamin D is important for building and maintaining strong bones. Calcium is necessary for bone structure, and vitamin D helps the body absorb calcium. Good dietary sources of calcium include dairy products, leafy green vegetables, and fortified foods such as orange juice. Vitamin D can be obtained through exposure to sunlight as well as dietary sources like fatty fish and fortified products.
However, it is important to note that diet alone may not provide enough calcium and vitamin D for optimal bone health, especially in individuals at risk for or with existing osteoporosis. In such cases, healthcare providers may recommend calcium and vitamin D supplements to ensure adequate intake.
In addition to a healthy diet, regular weight-bearing exercises, avoiding excessive alcohol consumption and smoking, and certain medications may be prescribed to prevent or treat osteoporosis. Considering all these factors together will provide the best approach to managing and reducing the risk of osteoporosis.
References:
– National Osteoporosis Foundation. (n.d.). Nutrition. Retrieved from https://www.nof.org/patients/treatment/nutrition/
– National Osteoporosis Foundation. (n.d.). Exercise for Strong Bones. Retrieved from https://www.nof.org/patients/fracturesfall-prevention/exercisesafe-movement/exercise-for-strong-bones/
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
34. What is the role of fall prevention in reducing the risk of fractures in individuals with osteoporosis?
Fall prevention plays a crucial role in reducing the risk of fractures in individuals with osteoporosis. People with osteoporosis have fragile bones, making them more susceptible to fractures, particularly in the event of a fall. Falls can lead to fractures of the hip, spine, wrist, and other bones, and these fractures can have severe consequences for individuals with osteoporosis.
There are several strategies that can be employed to prevent falls and minimize the risk of fractures. These include:
1. Regular exercise: Engaging in weight-bearing exercises, such as walking, dancing, or tai chi, can improve strength, balance, and coordination, reducing the likelihood of falls.
2. Home modifications: Ensuring a safe home environment by removing hazards, improving lighting, and installing grab bars in bathrooms can help prevent falls.
3. Medication review: Certain medications can increase the risk of falls. It is important for individuals with osteoporosis to review their medications, especially those that may cause dizziness or drowsiness, with their healthcare provider.
4. Vision check: Regular eye examinations can identify any vision problems that may contribute to falls.
5. Assistive devices: Using appropriate assistive devices, such as canes or walkers, can provide stability and aid in balance while walking.
By implementing these fall prevention strategies, individuals with osteoporosis can significantly reduce their risk of fractures and maintain their independence and quality of life.
References:
– National Osteoporosis Foundation. (n.d.). Exercises for Posture. Retrieved from https://www.nof.org/patients/fracturesfall-prevention/exercisesafe-movement/exercises-for-posture/
– Mayo Clinic. (2018). Fall prevention: Simple tips to prevent falls. Retrieved from https://www.mayoclinic.org/healthy-lifestyle/healthy-aging/in-depth/fall-prevention/art-20047358
35. Can osteoporosis be completely cured with treatment, or is it a lifelong condition?
Osteoporosis is a chronic condition that requires long-term management, and currently, there is no known cure for this disease. However, with appropriate treatment and lifestyle modifications, it is possible to slow down the progression of osteoporosis, reduce fracture risk, and improve overall bone health.
The primary goal of osteoporosis treatment is to prevent fractures and maintain bone density. Treatment may involve a combination of medication, exercise, dietary changes, and fall prevention strategies. Medications commonly used for osteoporosis treatment include bisphosphonates, denosumab, selective estrogen receptor modulators (SERMs), and hormone replacement therapy (HRT) for postmenopausal women.
It is important to note that treatment should be individualized based on factors such as age, sex, medical history, and fracture risk. Regular monitoring of bone density and response to treatment is also recommended to ensure optimal outcomes.
While the disease cannot be entirely reversed, proactive management can make a significant difference in preventing fractures and maintaining quality of life. Working closely with a healthcare provider, individuals with osteoporosis can develop a comprehensive treatment plan tailored to their specific needs.
References:
– National Osteoporosis Foundation. (n.d.). Osteoporosis Treatment. Retrieved from https://www.nof.org/patients/treatment/
– Mayo Clinic. (2020). Osteoporosis. Retrieved from https://www.mayoclinic.org/diseases-conditions/osteoporosis/diagnosis-treatment/drc-20351978
36. Are there any potential complications or long-term effects of osteoporosis treatment?
Yes, there can be potential complications or long-term effects associated with osteoporosis treatment. Some common treatments for osteoporosis, such as bisphosphonates, can cause side effects like gastrointestinal problems, including stomach pain, acid reflux, and nausea [Mayo Clinic. (2021). Bisphosphonates for osteoporosis: Possible side effects. https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/bisphosphonates/art-20044832]. In rare cases, long-term use of bisphosphonates might increase the risk of thigh bone fractures [National Osteoporosis Foundation. (2021). Bisphosphonates. https://www.nof.org/patients/treatment/bisphosphonates/]. Other medications used in osteoporosis treatment, such as hormone therapy, can have possible side effects like increased risk of blood clots, stroke, or breast cancer [Mayo Clinic. (2021). Hormone therapy: Is it right for you? https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/hormone-therapy/art-20046363]. However, it is important to note that the benefits of treatment usually outweigh the potential risks, and any concerns should be addressed with a healthcare professional.
37. How often should bone density tests be repeated to monitor the progression of osteoporosis?
The frequency of bone density tests can vary depending on various factors, including an individual’s age, medical history, and the severity of osteoporosis. Generally, it is recommended to have a bone density test every two years for individuals with osteoporosis or those at higher risk [National Osteoporosis Foundation. (2021). Testing for Osteoporosis. https://www.nof.org/patients/what-is-osteoporosis/testing-for-osteoporosis/]. However, for individuals with stable bone density and no significant changes in their risk factors, the frequency of testing can be extended to every three to five years [National Osteoporosis Foundation. (2021). Clinician’s Guide to Prevention and Treatment of Osteoporosis. https://www.nof.org/prevention/]. It is important to consult with a healthcare professional who can assess individual risk factors and provide personalized recommendations.
38. Are there any support groups or resources available for individuals living with osteoporosis?
Yes, there are numerous support groups and resources available for individuals living with osteoporosis. These resources offer guidance, education, and emotional support. Some notable organizations include the National Osteoporosis Foundation (NOF), which provides information, resources, and support through their website, including access to local support groups [National Osteoporosis Foundation. (2021). Support and Resources. https://www.nof.org/patients/support-and-resources/
]. The International Osteoporosis Foundation (IOF) is another organization that offers valuable resources, including pamphlets, educational materials, and online communities [International Osteoporosis Foundation. (2021). Resources. https://www.osteoporosis.foundation/resources
]. Additionally, many local hospitals or healthcare facilities may offer support groups specifically for individuals with osteoporosis. Connecting with these support groups can provide valuable insights and a sense of community for those living with the condition.
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
39. What steps can be taken to prevent osteoporosis in young adults?
Preventing osteoporosis begins early in life, and there are several steps young adults can take to reduce their risk:
1. Ensure a balanced diet: Consuming sufficient amounts of calcium-rich foods such as dairy products, leafy greens, and fortified foods helps promote strong bones [National Osteoporosis Foundation. (2021). Eating for Healthy Bones. https://www.nof.org/patients/fracturesfall-prevention/nutrition/
].
2. Get enough vitamin D: Adequate vitamin D levels are essential for calcium absorption. Spending time outdoors or taking supplements can help maintain sufficient levels [National Osteoporosis Foundation. (2021). Calcium and Vitamin D: What You Need to Know. https://www.nof.org/patients/treatment/calciumvitamin-d/].
3. Engage in weight-bearing exercises: Activities like walking, jogging, dancing, or weightlifting stimulate bone density and strength [National Osteoporosis Foundation. (2021). Exercise for Strong Bones. https://www.nof.org/patients/exercisesafe-movement/exercise-for-strong-bones/].
4. Avoid smoking and excessive alcohol consumption: Both smoking and excessive alcohol intake can negatively impact bone health [American Academy of Orthopaedic Surgeons. (2019). Alcohol and Bone Health. https://orthoinfo.aaos.org/en/staying-healthy/alcohol-and-bone-health/].
5. Maintain a healthy body weight: Being underweight can increase the risk of osteoporosis, so maintaining a healthy weight through balanced nutrition and regular exercise is important [International Osteoporosis Foundation. (2021). Lifestyle. https://www.osteoporosis.foundation/health-lifestyle].
It is advisable to consult with a healthcare professional to assess individual risk factors and develop a personalized preventive plan.
40. Is osteoporosis more common in certain populations or ethnic groups?
Yes, osteoporosis can vary in prevalence across different populations and ethnic groups. While osteoporosis affects both men and women, postmenopausal women are particularly susceptible due to the hormonal changes associated with menopause [NIH Osteoporosis and Related Bone Diseases National Resource Center. (2019). Osteoporosis in Men. https://www.bones.nih.gov/health-info/bone/osteoporosis/men]. Research suggests that Caucasian and Asian women are at a higher risk of developing osteoporosis compared to women from other ethnic backgrounds [National Osteoporosis Foundation. (2021). Osteoporosis in Different Populations. https://www.nof.org/patients/populations/]. This is partly attributed to differences in bone density, body structure, and genetic factors. However, it is important to note that osteoporosis can affect individuals from all populations and ethnic groups, and risk factors such as age, family history, and lifestyle choices play significant roles in determining an individual’s susceptibility to the condition [National Institutes of Health. (2021). Bone Health and Osteoporosis: A Report of the Surgeon General. https://www.ncbi.nlm.nih.gov/books/NBK45513/].
While I do cite reputable sources, I am not a medical professional. Please use professional medical advice when making any health-related decisions.
This comprehensive guide has shed light on a myriad of questions surrounding osteoporosis, an often underestimated condition with far-reaching consequences. By understanding the causes, risk factors, and prevention methods, we are empowered to take control of our bone health. Osteoporosis is not just a condition that affects the elderly; it can disrupt lives and rob us of our independence, vitality, and joy at any age. Therefore, it is crucial that we prioritize education and awareness, both for ourselves and our loved ones, to ensure early detection and effective management. Let us not underestimate the power of knowledge and the impact it can have on our lives. Share this guide with others, so that together we can take proactive steps towards a future with strong and healthy bones. After all, our bones are the foundation that supports us in everything we do. Let us invest in our bone health – for a life full of strength, resilience, and the freedom to embrace every moment with confidence.
References:
Mayo Clinic. (2021). Bisphosphonates for osteoporosis: Possible side effects. https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/bisphosphonates/art-20044832
National Osteoporosis Foundation. (2021). Bisphosphonates. https://www.nof.org/patients/treatment/bisphosphonates/
Mayo Clinic. (2021). Hormone therapy: Is it right for you? https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/hormone-therapy/art-20046363
National Osteoporosis Foundation. (2021). Testing for Osteoporosis. https://www.nof.org/patients/what-is-osteoporosis/testing-for-osteoporosis/
National Osteoporosis Foundation. (2021). Clinician’s Guide to Prevention and Treatment of Osteoporosis. https://www.nof.org/prevention/
National Osteoporosis Foundation. (2021). Support and Resources. https://www.nof.org/patients/support-and-resources/
International Osteoporosis Foundation. (2021). Resources. https://www.osteoporosis.foundation/resources
National Osteoporosis Foundation. (2021). Eating for Healthy Bones. https://www.nof.org/patients/fracturesfall-prevention/nutrition/
National Osteoporosis Foundation. (2021). Calcium and Vitamin D: What You Need to Know. https://www.nof.org/patients/treatment/calciumvitamin-d/
National Osteoporosis Foundation. (2021). Exercise for Strong Bones. https://www.nof.org/patients/exercisesafe-movement/exercise-for-strong-bones/
American Academy of Orthopaedic Surgeons. (2019). Alcohol and Bone Health. https://orthoinfo.aaos.org/en/staying-healthy/alcohol-and-bone-health/
International Osteoporosis Foundation. (2021). Lifestyle. https://www.osteoporosis.foundation/health-lifestyle
NIH Osteoporosis and Related Bone Diseases National Resource Center. (2019). Osteoporosis in Men. https://www.bones.nih.gov/health-info/bone/osteoporosis/men
National Osteoporosis Foundation. (2021). Osteoporosis in Different Populations. https://www.nof.org/patients/populations/
National Institutes of Health. (2021). Bone Health and Osteoporosis: A Report of the Surgeon General. https://www.ncbi.nlm.nih.gov/books/NBK45513/
Just a little heads up: some of the links on this site may be affiliate links, which means if you make a purchase through them, we might get a little kickback. But don’t worry, it won’t cost you a cent extra! Think of it as the universe secretly thanking us for helping you find a great deal. Your support keeps the good vibes flowing.
Additional Number-Associated References:
1. Mayo Clinic: “Osteoporosis: Overview.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
2. National Osteoporosis Foundation: “Causes of Osteoporosis.” Available at: https://www.nof.org/preventing-fractures/general-facts/causes/
3. Mayo Clinic: “Osteoporosis: Risk Factors.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
4. National Osteoporosis Foundation: “Genetics and Osteoporosis.” Available at: https://www.nof.org/preventing-fractures/general-facts/genetics-and-osteoporosis/
5. Harvard Health Publishing: “Age-related bone loss.” Available at: https://www.health.harvard.edu/womens-health/age-related-bone-loss
6. Mayo Clinic: “What is menopause?” Available at: https://www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397
7. National Osteoporosis Foundation: “Calcium and Vitamin D: What You Need to Know.” Available at: https://cdn.nof.org/wp-content/uploads/2015/12/calciumvitaminD_ingredients.pdf
8. Mayo Clinic: “Vitamin D: Important for Bone Health.” Available at: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/vitamin-d-deficiency/faq-20058397
9. National Osteoporosis Society: “Risk Factors and Prevention.” Available at: https://theros.org.uk/information-and-support/preventing-osteoporosis/risk-factors-and-prevention/
10. Mayo Clinic: “Osteoporosis: Medications that can cause bone loss.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/medications-that-can-cause-bone-loss/art-20045758
11. National Osteoporosis Foundation: “What is Osteoporosis?” Available at: https://www.nof.org/preventing-fractures/general-facts/what-is-osteoporosis/
12. Mayo Clinic: “Osteoporosis: Complications.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
13. National Osteoporosis Foundation: “Osteoporosis Testing: What You Need to Know.” Available at: https://www.nof.org/preventing-fractures/general-facts/osteoporosis-testing/
14. Mayo Clinic: “Bone density test.” Available at: https://www.mayoclinic.org/tests-procedures/bone-density-test/about/pac-20385273
15. National Osteoporosis Foundation: “Osteoporosis Diagnosis.” Available at: https://www.nof.org/preventing-fractures/general-facts/diagnosis/
16. Mayo Clinic: “Osteoporosis diet plan: What to eat and avoid.” Available at: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/osteoporosis-diet/art-20045012
17. National Osteoporosis Foundation: “Nutrition.” Available at: https://www.nof.org/preventing-fractures/nutrition/
18. Mayo Clinic: “Exercise for Healthy Bones.” Available at: https://www.mayoclinic.org/healthy-lifestyle/fitness/in-depth/exercise/art-20047414
19. National Osteoporosis Society: “Exercise.” Available at: https://theros.org.uk/information-and-support/living-with-osteoporosis/exercise/
20. Mayo Clinic: “Hormone therapy and Osteoporosis.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/hormone-therapy/art-20045776
21. National Osteoporosis Foundation: “Medication.” Available at: https://www.nof.org/patients/treatment/medicationadherence/
22. Mayo Clinic: “Osteoporosis Medications: Balancing Benefits and Risks.” Available at: https://www.mayoclinic.org/healthy-lifestyle/medication-use/in-depth/osteoporosis-drugs/art-20394908
23. National Osteoporosis Foundation: “Bisphosphonates.” Available at: https://www.nof.org/patients/treatment/medicationadherence/bisphosphonate-therapy/
24. Mayo Clinic: “Calcitonin (Fortical, Miacalcin).” Available at: https://www.mayoclinic.org/drugs-supplements/calcitonin-fortical-miacalcin-nasal-route/side-effects/drg-20074702
25. National Osteoporosis Foundation: “SERMs.” Available at: https://www.nof.org/patients/treatment/medicationadherence/serms/
26. Mayo Clinic: “Parathyroid Hormone (PTH) and Teriparatide.” Available at: https://www.mayoclinic.org/drugs-supplements/teriparatide-subcutaneous-route/side-effects/drg-20067673
27. National Osteoporosis Foundation: “Alternative Management Techniques.” Available at: https://www.nof.org/patients/treatment/medicationadherence/alternative-management-techniques/
28. Mayo Clinic: “Smoking and Osteoporosis: Can Smoking Increase Your Risk?” Available at: https://www.mayoclinic.org/healthy-lifestyle/quit-smoking/expert-answers/smoking-and-osteoporosis/faq-20058119
29. National Osteoporosis Foundation: “Alcohol and Osteoporosis.” Available at: https://www.nof.org/patients/treatment/alcohol-and-osteoporosis/
30. Mayo Clinic: “Caffeine and Osteoporosis: Do They Mix?” Available at: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/osteoporosis-diet/faq-20058128
31. National Osteoporosis Foundation: “Rheumatoid Arthritis and Osteoporosis.” Available at: https://www.nof.org/patients/treatment/related-conditions/rheumatoid-arthritis-and-osteoporosis/
32. Mayo Clinic: “Osteoporosis Surgery.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/diagnosis-treatment/drc-20351973
33. National Osteoporosis Foundation: “Lifestyle Changes.” Available at: https://www.nof.org/patients/treatment/lifestyle-changes/
34. Mayo Clinic: “Fall prevention: Simple tips to prevent falls.” Available at: https://www.mayoclinic.org/healthy-lifestyle/healthy-aging/in-depth/fall-prevention/art-20047358
35. National Osteoporosis Foundation: “Is Osteoporosis Curable?” Available at: https://www.nof.org/patients/treatment/is-osteoporosis-curable/
36. Mayo Clinic: “Osteoporosis Treatment: Long-term drug therapy.” Available at: https://www.mayoclinic.org/healthy-lifestyle/medication-use/in-depth/osteoporosis-treatment/art-20046869
37. National Osteoporosis Foundation: “Monitoring Osteoporosis Treatment.” Available at: https://www.nof.org/patients/treatment/medicationadherence/monitoring-osteoporosis-treatment/
38. Mayo Clinic: “Coping and Support.” Available at: https://www.mayoclinic.org/diseases-conditions/osteoporosis/diagnosis-treatment/drc-20351973
39. National Osteoporosis Foundation: “Preventing Osteoporosis.” Available at: https://www.nof.org/preventing-fractures/prevention/
40. Mayo Clinic: “Ethnicity and Osteoporosis: What’s the Connection?” Available at: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/osteoporosis/faq-20058335